Root Canal
Endodontic treats roots of the tooth within your jaw. In this hollow space is living tissue called the "dental pulp" containing blood vessels and nerves. It is similar to most other tissue in your body except that it is very sensitive and is surrounded by the hard tissue of the tooth.

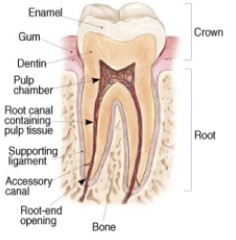
Endodontics specifically treats problems associated with the inside of the tooth. To fully understand this, it helps to know a little about the anatomy of a tooth. Every tooth is covered on the outside by a very hard, white, material called enamel. Inside of this is a deeper material called dentin, also hard but less so than enamel. At the center of the dentin is a hollow space than extends from the “crown” end of the tooth, or the part that you see in the mouth, all the way down to the tips of the “Endo” is the Greek word for “inside”, and “odont” is Greek for tooth. Endodontic treats roots of the tooth within your jaw. In this hollow space is living tissue called the “dental pulp” containing blood vessels and nerves. It is similar to most other tissue in your body except that it is very sensitive and is surrounded by the hard tissue of the tooth. When you are very young, this tissue actually forms the tooth around itself. Once your tooth is fully formed, this tissue does not play as active of a role but remains to give you feedback on when you are biting too hard, and when things are hot or cold etc. Since this tissue is not critical to your tooth during your adult life, the tooth can actually survive almost unchanged without this tissue.
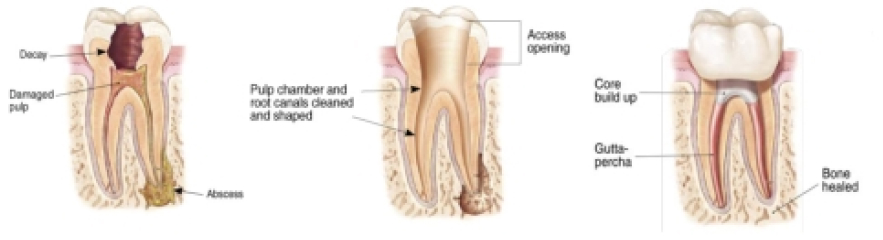
One characteristic of this tissue is that it has a somewhat reduced ability to heal itself when it becomes injured. Your blood is the primary source of cells involved in healing and repairing inflammation and injury . Since the only way for your blood supply to get to the tissue in your tooth is through tiny openings in the end of the roots, inflammation and increased pressure in this tissue are harder to correct. The injuries that occur to this tissue from cavities, deep fillings, cracks, and trauma tend to add up over a lifetime, and can reach a point when the body can no longer eliminate the inflammation. The inflammation then causes pain and discomfort, and if left untreated, usually leads to death of this tissue. Once the tissue dies, an infection usually follows which can spread out the root ends and cause a jaw infection or “abscess”. Abscesses are usually related to pain and swelling, but can exist without any symptoms other than showing up on a dental X-ray film.
To solve this problem, our Austin endodontist removes the inflamed or infected tissue and cleans the hollow space in the tooth to remove all remnants and bacteria present. Once this space is emptied, cleansed, and shaped, it can be filled with a biocompatible material to seal this space from any entry of bacteria in the future.
How is the Treatment Accomplished?
An examination is accomplished prior to treatment to review your clinical signs and symptoms and any relevant X-ray films. You will go over your health history with our Austin endodontist and the financial and insurance arrangements for treatment will be discussed. Even if you have been examined by your general dentist, it will also need to be done by your endodontist, for both legal and ethical reasons, as the provider of your care. This examination is either accomplished at a separate appointment before treatment is scheduled, or in cases where your general dentist feels certain about the nature of care needed, time can be incorporated into the treatment appointment to allow verification of diagnosis and completion of information gathering without a separate visit. Once the treatment phase has begun, the affected area of your mouth is completely numbed with local anesthetic, just like when you have a filling. A small opening is made through the chewing surface of the tooth, filling, or crown, to gain access to the hollow “pulp” space. Small cleaning instruments are used to remove the contents of this space and smooth and shape the internal walls. Disinfecting solutions are used to help remove any bacteria present. Once the endodontist is satisfied that the space is clean, a filling material is inserted to completely seal the internal space. The most common material used is a naturally occurring product called “gutta percha”, used because of it’s biocompatibility and ability to be softened and conform to all of the internal shapes of the tooth. Once this cleaning and filling has occurred, either your endodontist or your general dentist will then place a filling material in the opening created on the chewing surface of the tooth to strengthen and seal the tooth structure. If the tooth does not already have a crown, it is usually recommended that one be placed by your general dentist to protect the tooth, since once the hollow space has been enlarged and cleaned, the tooth is more susceptible to cracking in future years. Where a crown already exists on the tooth, the root canal procedure in most cases does not damage the crown and a filling in the chewing surface can seal and maintain the crown for many years. In some cases, if a significant amount of tooth structure is missing or damaged, a “post” or reinforcing rod is placed into part of the hollow space created by the root canal treatment to help reinforce the filling that will be placed. The decision on whether or not a post is needed is made on a case by case basis. This reinforcement with fillings and posts may be done by your general dentist or your endodontist, depending on your general dentist’s preferences.
If the internal space does not become contaminated in the future by new decay, leaking fillings, or cracks, the root canal treatment can last a lifetime. Studies show long term success with root canals to be 80-90% or better.
Besides the structural problems listed above that can recontaminate the internal space, sometimes teeth have internal areas difficult to find and access during treatment. Some roots can also have extra “canals” or hollow spaces that are not expected and not found during the first treatment. Some of these problems can cause a recurrence of pain or swelling and a second treatment to re-open and search for causes is necessary. If this is needed, the treatment is often similar to the first root canal, but may require added care and time to get through metal fillings, posts, and the previous root canal filling material.
Occasionally during endodontic treatment, calcifications or blockages prevent the complete cleaning of the internal spaces. Also when retreatment of a previous root canal is needed, some of the posts and dental work placed after the first root canal can block access to the internal space in such a way that they cannot be safely bypassed. In some cases bacteria on the external surface of the root ends and in the jaw may not have been eliminated by the internal root canal procedure and are resistant to your body’s ability to eliminate them. In these situations, an alternative approach to cleaning and sealing the root end is considered. By making an incision in the gum tissue next to the tooth, the gum can be moved aside and the root approached directly from the side of the tooth. In this way, any infection around the root is cleaned and the root end is sealed from the opposite end. The gum tissue is replaced in it’s original position with a few sutures or “stitches” and the area followed over time for healing.
Cleaning or re-cleaning from the top of the tooth through the inside space is always considered the preferred treatment because there is a better chance of cleaning the entire length of the tooth. When this is not possible however, the surgical approach discussed above still has a good chance of success. The surgery itself is usually as easily tolerated as a conventional root canal procedure. As with any surgery, some soreness and swelling may occur over the first few days following the treatment. A more in depth discussion with your endodontist can help you make the decision on which approach is best suited for your individual case needs.
